
Innovation
We can do better to prevent, diagnose, and manage hypertensive disorders of pregnancy
Last Updated on March 11, 2025
INNOVATION FOR HYPERTENSIVE DISORDERS OF PREGNANCY STARTS WITH PRENATAL AND POSTPARTUM CARE
Prenatal and postpartum care – as it’s generally practiced in the United States – hasn’t changed much in over 50 years. First developed primarily to diagnose preeclampsia (then called "toxemia"), prenatal visits include peeing in a cup, weighing mom, and taking her blood pressure, over the course of 12 to 14 prenatal visits, spaced one month apart until the third trimester when visits increase to once a week in the last month. Following delivery, a single postpartum visit at 6 weeks clears mom to resume normal activities and offers birth control (contraceptives).
Innovations and disruptive technologies in maternity care are desperately needed to better prevent, diagnose, and manage hypertensive disorders of pregnancy. Research, development, and implementation of newer models of care are, in some places, starting to be realized.
A postpartum visit within one week is now recommended as part of recognizing the physical and mental challenges in the “4th trimester” – the three months following delivery, especially important for mothers who experienced any kind of hypertension or medical complications. The 4th Trimester Project has developed several valuable resources that can help providers better serve their postpartum patients.
Aspirin, while far from being a cure-all, may help some women prevent or delay the onset of preeclampsia and is more widely prescribed to those at high or moderate risk.
Group care, telehealth, and connected care are models being tested in various settings to provide more customized prenatal care. Read more about those below, under Glossary. More advanced biomarkers are in development that can predict a woman’s risk of preeclampsia or diagnose it more accurately and earlier than traditional methods. We are active proponents of these innovations in obstetric care on Capitol Hill and elsewhere.
The Preeclampsia Foundation plays an active and vocal role in these innovations. Our goal is to disrupt inadequate healthcare practices, improve the patient experience, and eliminate disparities and health inequities.
Examples of our work
- PRIME research network, funded by the Preeclampsia Foundation, studied text-based, remote BP monitoring during the postpartum period at three sites across the country.
- Heart Health 4 Moms (HH4M), a virtual intervention to reduce cardiovascular risk and improve self-efficacy in preeclampsia survivors, and Health After Preeclampsia: Patient and Provider Engagement (HAPPPEN) study, synthesized and reported the experiences of five postpartum clinics. Both were designed to provide specialty care for preeclampsia survivors.
- The Cuff Kit® program, which we quickly mobilized during the COVID-19 pandemic to get self-measured blood pressure cuffs into the hands of pregnant and postpartum patients. Telehealth services were not all equipped to provide women with the blood pressure monitors they needed for at-home monitoring.
- Our work on preeclamspia biomarkers, which included convening thought leaders and stakeholders and launching a call to action for numerous stakeholders, calling for specific and accurate tests to predict and diagnose preeclampsia and related disorders of pregnancy.
GLOSSARY
Often under the brand name Centering Pregnancy®, group care allows a patient to meet with a group of other patients with similar due dates to share and learn relevant information, check blood pressure, and address medical and social services needs. The woman has time alone with her maternity care provider to check fetal heart rate and discuss any unique or sensitive issues. This ad hoc community often create bonds that extend beyond delivery and encourage peer support for parenting and newborn issues.
Telehealth allows a patient to meet with her healthcare provider through a phone or video call. The patient checks her own vital signs such as blood pressure and shares this information with her provider. Under the COVID-19 pandemic, we saw a surge in telehealth usage as regulations were loosened and women were either afraid to physically go to hospitals or clinics and providers sought to minimize unnecessary exposure.
Connected care usually means a patient has a reduced number of individual appointments and in between uses remote technology to assess her BP and other vital signs which are often automatically transmits to her provider. A nurse or some system of assessment ensures those data are monitored and appropriate responded to. An example is this program in Louisiana.
Research, development and marketing of biomarkers to predict and diagnose preeclampsia have accelerated in recent years. In the United Kingdom and other areas of the world, commercial tests are already on the market. Utilizing proteomics, metabolomics, and other analytes, molecular biomarkers have the potential to finally define preeclampsia as one or more specific conditions, rather than its current status as a syndrome because of the loose collection of “clues” that makes diagnosis and treatment often ambiguous, even to experts.
Related Articles
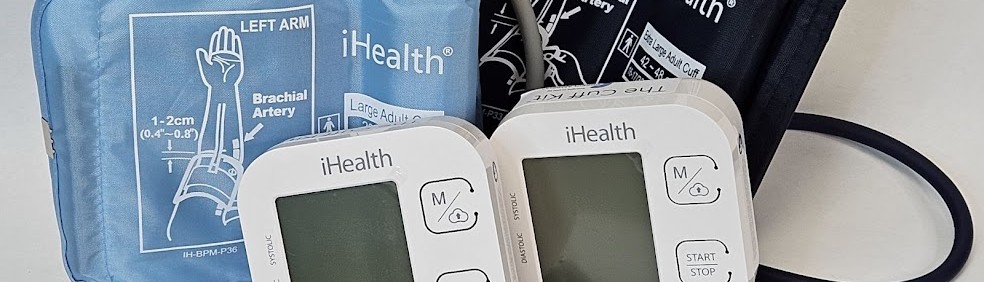
Congratulations on receiving your brand new Cuff Kit®! Want to learn more about how to use your iHealth Track device? Here are some handy videos and links to get you started. Unpacking and using...

Nurses play a vital role in detecting preeclampsia and caring for patient before, during, and beyond pregnancy.

A key component needed in the fight against preeclampsia is the development of tests for simple, rapid, and accurate diagnosis and prediction through the development and adoption of biomarkers.

As a first step to address the need for self-monitored blood pressure, the Preeclampsia Foundation started providing the Cuff Kit® in June 2020 to women at highest risk of developing preeclampsia and...

Every woman should be able to check her own blood pressure at home.

For more on the Preeclampsia Foundation's work to amplify all research related to biomarkers for improved prediction and diagnostic tools, please visit https://preeclampsia.org/biomarkers. INDIANAPOL...

GAP—SPIRIN campaign gets low-dose aspirin to those most at risk to help close the maternal health gap in preeclampsia ________ NEW YORK, January 23, 2025/PRNewswire/ – In recognition of...
1732072344.png)
While the Preeclampsia Foundation has been championing patient advocacy and representation for all families affected by hypertension in pregnancy throughout our 25 year history, we recognized the uniq...

Washington, DC – April 11, 2024 – On April 10, one day before the start of Black Maternal Health Week, the Preeclampsia Foundation in partnership with Thermo Fisher Diagnostics held a Hill...

Recently, I came across a social media post calling attention to the global maternal health crisis from a Black woman’s perspective. Someone responded to the post asking, “What’s rac...
