
Cuff Kit® to protect moms and babies
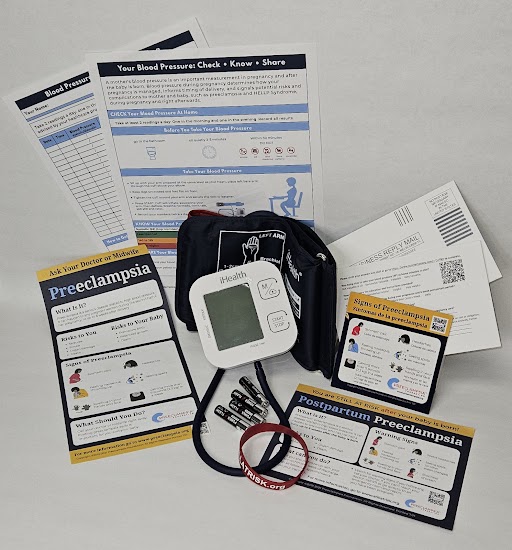
Give moms the tools to monitor for hypertensive disorders of pregnancy with the Cuff Kit®
Last Updated on October 23, 2025
 The Need
The Need
Preeclampsia can strike quickly. Give new and expectant moms the best tool for early detection of hypertensive disorders with the Cuff Kit®. Pregnancy-related hypertensive disorders, including preeclampsia, eclampsia, HELLP syndrome, chronic hypertension, gestational hypertension, and superimposed preeclampsia, affect up to one in 12 pregnancies annually and can lead to life-long cardiovascular complications.
Brought to you by the trusted team at the Preeclampsia Foundation, the Cuff Kit® includes a pregnancy-validated monitor with evidence-based education materials to ensure every patient knows the symptoms and signs of disease and reports it back to you! Pregnant patients may not be attending all of their prenatal and postpartum visits in person. This means that blood pressure screening, recommended throughout and after pregnancy[i], proteinuria assessments, and a review of signs and symptoms may not happen for thousands of women each day.
Helping patients accurately self-monitor blood pressure at home and act fast on credible data can be a life-saver.
The Preeclampsia Foundation Cuff Kit® is a trusted, pregnancy-validated tool to make self-measured blood pressure cuffs with educational materials available to all pregnant and postpartum women at risk of developing preeclampsia and other hypertensive disorders of pregnancy – especially to our most vulnerable populations.
The kit includes:
- A pregnancy-validated automatic blood pressure monitoring device with batteries[ii]
- Instructions sheet with access to online video tutorial
- Blood pressure tracking log
- Signs and symptoms of preeclampsia tearsheet
- Signs and symptoms of postpartum preeclampsia education sheet
- Signs and symptoms magnet
- “Still at Risk” rubber bracelet
- Patient feedback link
All Cuff Kit® materials come in dual English/Spanish, but are also available in Arabic, Burmese, Chinese (simplified), Haitian Creole, French, Kirundi, Pashto, Somali, Swahili, Ukrainian. If you are interested in materials in any of these languages, please email our team at cuffkit@preeclampsia.org.
Already have cuffs but need the educational materials? Introducing the "Check Know Share" Self-Measured Blood Pressure Education Kit
Does your facility already have blood pressure cuffs, but not the patient education materials on preeclampsia signs and symptoms or how to take their own blood pressure? We are now offering a second great option for your pregnancy and postpartum self-measured blood pressure program through our "Check Know Share" Self-Measured Blood Pressure Education Kit! Great for programs that are already accessing blood pressure cuffs through other means, this wrap-around kit gives you everything your patient needs to know how to accurately take their blood pressure:
- Instructions sheet with access to online training video and patient feedback link
- Paper blood pressure tracking log
- Signs and symptoms of preeclampsia sheet
- Signs and symptoms of postpartum preeclampsia education sheet
- Signs and symptoms magnet
- “Still at Risk” postpartum rubber alert bracelet
Purchase the SMBP Education Kits
Interested in providing the Cuff Kit® to your patients?
Participating providers must be able to:
- Quickly and readily communicate with participating patients, utilizing telehealth as needed;
- Prioritize distribution to highest risk, especially vulnerable women with lower ability to procure their own BP cuff (i.e., Individual risk factors include chronic hypertension, history of preeclampsia, obesity, age (35+), autoimmune disorders; as well as population-level risk factors such as black, Native American, or rural women);
- Commit to provide quarterly feedback to help us assess the impact of this initiative. Please see our questions here, so you can implement systems to collect this data.
Have questions? Email our team at cuffkit@preeclampsia.org.
The Cuff Kit® Project: Our Strategic Plan
The ability for all women to access healthcare during and after pregnancy has been further challenged by COVID-19, but the application of home monitoring and telehealth as an important option has garnered considerable attention. (Check out one woman's story of how a self-measured blood pressure cuff helped her detect her own preeclampisa as featured on CNN Health.) Although the Cuff Kit is an important and urgent first step, our view of this solution extends beyond the emergency response to COVID-19. There is immediate need to fund projects related to this entire scope of work:
- Purchase and provide additional Cuff Kits®, coupled with telehealth options, to support high-risk, low resource women across the US.
- Collect data, analyze and publish results of self-monitored and remote blood pressure measurement programs in pregnancy and the postpartum period. Outcome measurements should include maternal and neonatal mortality and morbidity, healthcare costs, impact on racial disparities.[iii]
- Technical evaluation and validation of current home-monitoring devices/services for use in pregnancy, with secondary validation for preeclamptic pregnancies.[iv]
- Assess policies and drive regulatory and clinical changes, as needed, to add self-monitored and remote blood pressure measurements to obstetrics standards of care.
- Advocacy efforts with public and private insurers to universally reimburse for home-monitored blood pressure measurement for all pregnant and postpartum women.
[i] JAMA. 2017;317(16):1661-1667. doi:10.1001/jama.2017.3439
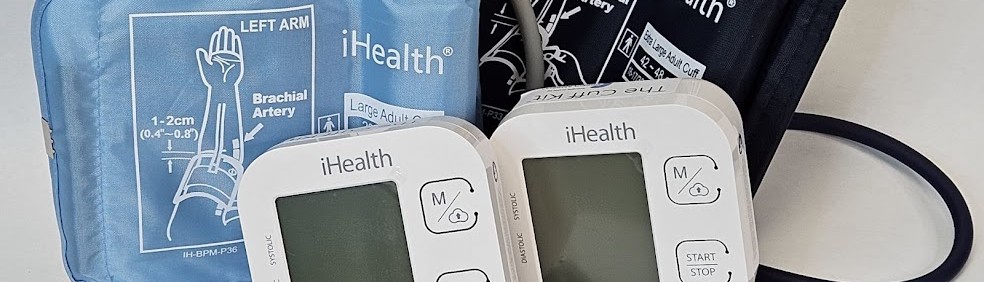
[ii] Cuff Kits utilize the Andon iHealth Track blood pressure monitor device, which has been independently validated for home blood pressure monitoring in pregnant populations by Stride BP, a joint initiative with the European Society of Hypertension, International Society of Hypertension, and the World Hypertension League.
[iii] Oral presentation at the 39th Annual Pregnancy Meeting of the Society for Maternal-Fetal Medicine, Las Vegas, NV, Feb 11-16, 2019. https://doi.org/10.1016/j.ajog.2019.05.011
[iv] Bello N. Hypertension. 2018;71:326-335. DOI: 10.1161/HYPERTENSIONAHA.117.10295
Related Articles
Congratulations on receiving your brand new Cuff Kit®! Want to learn more about how to use your iHealth Track device? Here are some handy videos and links to get you started. Unpacking and using...

Nurses play a vital role in detecting preeclampsia and caring for patient before, during, and beyond pregnancy.

A key component needed in the fight against preeclampsia is the development of tests for simple, rapid, and accurate diagnosis and prediction through the development and adoption of biomarkers.

Every woman should be able to check her own blood pressure at home.

Order our Ask About Aspirin Rack Card. Aspirin can prevent the formation of blood clots. This can make aspirin useful in treating or preventing some conditions like heart attacks and st...

Preventing and managing high blood pressure with healthy lifestyle behaviors are at the center of updated clinical guidelines published this week in the American Heart Association (AHA) peer-reviewed...

Hypertensive disorders of pregnancy are a leading cause of maternal death in the state of Indiana. To address this critical issue, the Indiana Hospital Association is teaming up with the Preeclampsia...

Recientemente, me encontré con una publicación en las redes sociales señalando la crisis de salud maternal desde la perspectiva de una mujer negra. Una persona respondió a...

For more on the Preeclampsia Foundation's work to amplify all research related to biomarkers for improved prediction and diagnostic tools, please visit https://preeclampsia.org/biomarkers. INDIANAPOL...

GAP—SPIRIN campaign gets low-dose aspirin to those most at risk to help close the maternal health gap in preeclampsia ________ NEW YORK, January 23, 2025/PRNewswire/ – In recognition of...


