
Maternal Early Warning Signs: Preeclampsia
States and healthcare systems that are making a concerted effort to respond to the alarming maternal mortality and morbidity rate in this country are discovering something important. Neglect, delayed diagnosis, and inadequate management contributed to poor outcomes in women with preeclampsia and other hypertensive crises in pregnancy[1].
If you’re a healthcare provider, you should know that protocols for early warning systems, including a list of criteria that indicate urgent bedside evaluation, have been created to facilitate more timely recognition and more effective therapeutic intervention[2]. While we don’t yet truly understand the entire cause of preeclampsia and there is no sure fire prevention or treatment, much can be done with what we do know today.
Protocols for early warning systems, including a list of criteria that indicate urgent bedside evaluation, have been created to facilitate more timely recognition and more effective therapeutic intervention[2]. While we don’t yet truly understand the entire cause of preeclampsia and there is no sure fire prevention or treatment, much can be done with what we do know today.
Numerous guidelines, toolkits, and bundles have been created specifically to address the preventable morbidity and mortality associated with preeclampsia[3]. While somewhat an oversimplification, it really boils down to just five things:
- Recognize the symptoms
- Control blood pressure
- Prevent seizures
- Deliver at the optimal time
- Ensure postpartum surveillance
Maternal Early Warning Systems (MEWS), now operationalized as a bundle[4], cite the following criteria as requiring immediate bedside evaluation:
|
Systolic BP (mm Hg) |
<90 or >160 |
|
Diastolic BP (mm Hg) |
>100 |
|
Heart rate (beats per minute) |
<50 or >120 |
|
Respiratory rate (breaths per minute) |
<10 or >30 |
|
Oxygen saturation (%) |
<95 |
|
Oliguria, mL/hr for >=2 hours |
<35 |
|
Maternal agitation, confusion, or unresponsiveness |
|
|
Patient with preeclampsia reporting a non-remitting headache or shortness of breath |
The current definition of preeclampsia includes blood pressure of 140/90 or greater and protein in the urine OR one or more indications of other organ failures (thrombocytopenia, liver, renal, pulmonary, cerebral or vision)[5]. HELLP syndrome, a particularly dangerous variant, often presents without alarming blood pressures, but epigastric pain, vomiting and flu-like symptoms may be the hallmarks of the liver failure usually underway. Given this, it’s easy to see why MEWS is optimally organized to ensure that women like Lauren Bloomstein do not die from preeclampsia.
What’s less obvious is the role of patients and their family members in this MEWS world. The Joint Commission issued Sentinel Event Alert #44 in January 2010. Among several preeclampsia-specific calls to action to address preventable maternal death, the alert noted the need to identify specific triggers for responding to changes in the mother’s vital signs and clinical condition. It also emphasized the need to use protocols for responding to these changes. One protocol is to inform the patient and family how to seek assistance when they have concerns about a patient’s condition. (This and other protocols have now been codified and there are some excellent implementation practices provided by the Council on Patient Safety in Women’s Healthcare.)
But how is a patient to know what she should be alert to and consider worthy of engaging her providers?
This is where deliberate, effective and, where possible, evidence-based patient education tools and techniques become critical. Lamaze instructors are in an excellent position to partner on these life-saving strategies. The Preeclampsia Foundation advocates for patient education to be offered throughout the prenatal care period and upon discharge.
Women must be taught the symptoms of preeclampsia (see box below), understanding that these do not lead to a certain diagnosis, but are causes for immediate follow up. If she’s in the hospital or birth center before, during, or after childbirth, she or her family must advocate for immediate bedside assistance to evaluate her vital signs, call for blood work or further testing, and determine if her care must be escalated. Hypertensive disorders like preeclampsia and HELLP syndrome can worsen quickly!
Adult learning techniques and evidence-based tools like the Preeclampsia Foundation’s tear sheet, clinic poster, and video can aid care providers, childbirth educators, doulas. More important than any tool is the attitude that care providers have toward patient education. It should be deemed as important at all levels of healthcare (administration to med techs). And it should reflect the fact that all of us learn differently, with varying amounts of health literacy and different perceptions of our roles within the healthcare environment (i.e., is the doctor the defacto expert or does the patient have a proactive role to play?). This is an opportunity early in a woman’s life course to empower the mother to understand and become an active participant in her and her new baby’s health, a lifelong skill, and increasingly a necessity as we are called to navigate a complex healthcare system.
More information about Maternal Early Warning Signs, and especially patient education techniques and tools, is available through this webinar audio recording and slide deck sponsored by the Council on Patient Safety in Women’s Healthcare. Lamaze Certified Childbirth Educator Jessica Deeb, MS, RN, WHNP-BC, IBCLC, LCCE, joined me as co-presenter, bringing valuable tips about effective adult learning.
[1] Main, Elliott K., McCain, Christy L., Morton, Christine H., Holtby, Susan, Lawton, Elizabeth S., “Pregnancy-Related Mortality in California: Causes, Characteristics, and Improvement Opportunities.” Obstetrics & Gynecology. April 2015.
[2] Mhyre, Jill M., D’Oria, Robyn, Hameed, Afshan B., Lappen, Justin R., Holley, Sharon L., Hunter, Stephen K., Jones, Robin L., King, Jeffrey C., D’Alton, Mary E., “The Maternal Early Warning Criteria: A Proposal from the National Partnership for Maternal Safety.” Obstetrics & Gynecology. October 2014.
[3]“Hypertension in Pregnancy.” The American College of Obstetricians and Gynecologists. 2013.
[3]Main, Elliott K., McCain, Christy L., Morton, Christine H., Holtby, Susan, Lawton, Elizabeth S., “Pregnancy-Related Mortality in California: Causes, Characteristics, and Improvement Opportunities.” Obstetrics & Gynecology. April 2015.
[4] Mhyre, Jill M., D’Oria, Robyn, Hameed, Afshan B., Lappen, Justin R., Holley, Sharon L., Hunter, Stephen K., Jones, Robin L., King, Jeffrey C., D’Alton, Mary E., “The Maternal Early Warning Criteria: A Proposal from the National Partnership for Maternal Safety.” Obstetrics & Gynecology. October 2014.
[5] “Hypertension in Pregnancy.” The American College of Obstetricians and Gynecologists. 2013.
Related Articles
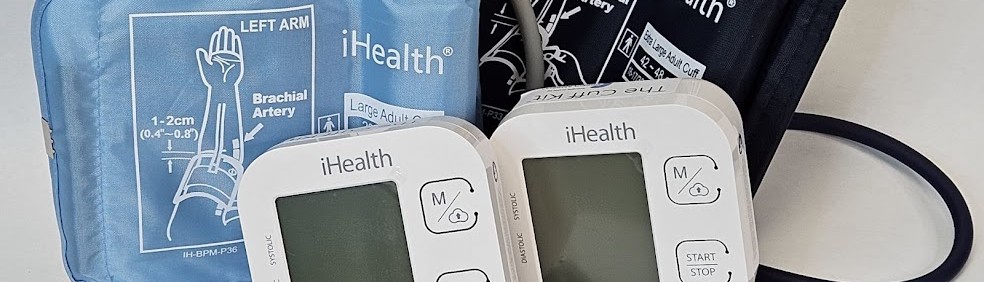
Congratulations on receiving your brand new Cuff Kit®! Want to learn more about how to use your iHealth Track device? Here are some handy videos and links to get you started. Unpacking and using...

Nurses play a vital role in detecting preeclampsia and caring for patient before, during, and beyond pregnancy.

A key component needed in the fight against preeclampsia is the development of tests for simple, rapid, and accurate diagnosis and prediction through the development and adoption of biomarkers.

Preeclampsia can strike quickly. Give new and expectant moms the best tool for early detection of hypertensive disorders with the Preeclampsia Foundation Cuff Kit® - a pregnancy-validated monitor wit...

Every woman should be able to check her own blood pressure at home.

Preventing and managing high blood pressure with healthy lifestyle behaviors are at the center of updated clinical guidelines published this week in the American Heart Association (AHA) peer-reviewed...

Hypertensive disorders of pregnancy are a leading cause of maternal death in the state of Indiana. To address this critical issue, the Indiana Hospital Association is teaming up with the Preeclampsia...

Recientemente, me encontré con una publicación en las redes sociales señalando la crisis de salud maternal desde la perspectiva de una mujer negra. Una persona respondió a...

For more on the Preeclampsia Foundation's work to amplify all research related to biomarkers for improved prediction and diagnostic tools, please visit https://preeclampsia.org/biomarkers. INDIANAPOL...

GAP—SPIRIN campaign gets low-dose aspirin to those most at risk to help close the maternal health gap in preeclampsia ________ NEW YORK, January 23, 2025/PRNewswire/ – In recognition of...
