
trauma informed therapy
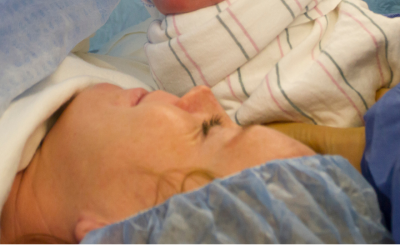
How can I heal after a traumatic birth experience?
Shattered Expectations: What happens after the unexpected?
You may have received the unexpected news that you have preeclampsia or another hypertensive disorder of pregnancy. Maybe labor complications led to an emergency c-section or a medical emergency, which was not how you envisioned your birth experience. Or you developed postpartum preeclampsia, eclampsia, or HELLP syndrome. Your baby may have had a NICU stay, or you are experiencing loss. Maybe you experienced postpartum depression or anxiety during the 4th trimester that left you feeling disconnected; became deprived of sleep, food, and/or water; or unable to control intrusive thoughts (amongst other uncomfortable and sometimes scary symptoms).
Any one of these situations might lead to trauma, which can be defined as the subjective experience of something extremely distressing that overwhelms our ability to cope as we normally would, and therefore be considered a traumatic birth experience. "A traumatic childbirth experience refers to a woman's experience of interactions and/or events directly related to childbirth that caused overwhelming distressing emotions and reactions; leading to short and/ or long-term negative impacts on a woman's health and wellbeing." ¹
If we were to ask 10 experts what their definition of trauma is, we would probably receive 10 different answers. That said, there are some pretty consistent overlapping pillars that you can count on for clarity when it comes to trauma.²
- Trauma is something that feels too much, too fast, and too soon that psychologically overwhelms us.
- It occurs when normal expectations in life are shattered by overwhelming force.
Let’s break down that last example together. We expect that when we cross the street at a crosswalk, we won’t get hit by a car. In the same way, when we invest time and effort into a relationship, we expect that trust to be mutual, not broken by betrayal or harm. When those basic expectations are violated, the result can be deeply unsettling. That’s trauma.
Similarly, when we’ve been told our whole lives as women that our bodies are “made” to get pregnant, give birth, and become mothers, and we’ve grown up hearing stories of “easy” pregnancies from the women around us, we expect things to go smoothly for us, too. That’s the hope, and what we all deserve. But sometimes, maybe more often than we realize, that’s not how it unfolds. For some, the journey includes infertility. For others, it’s miscarriage, high-risk pregnancies, birth complications, or postpartum struggles that no one warned them about. And that gap between expectation and reality?
Shattered expectations. Trauma.
And just as we may not be prepared for something to go wrong in the pregnancy or birth process, whether traumatic or not, we’re often just as unprepared for the emotional and mental health challenges that can follow. Many don’t know what’s happening, let alone where to turn for help.
So how do I heal after a traumatic birth experience?
Remember, you're not alone. You're doing the best you can. One place to start is to find a maternal mental health expert. Maternal mental health providers can make a big difference in helping you improve your mental health and process birth trauma. These therapists have specialized training and experience in PMADS (Perinatal Mood and Anxiety Disorders), birth trauma, matrescence (the transition into motherhood), and more. They are here to hold and support mothers who may be depressed, grieving, exhausted, or anxious and gently guide them toward healing and hope.
You can search for a perinatal mental health therapist on these specialized directories:
Perinatal providers can also support non-birthing parents, with many specializing in support for fathers and partners, as well. It’s a crucial reminder that about 1 in 10 men are at risk of developing postpartum depression.
"Psychological birth trauma and childbirth-related posttraumatic stress disorder represent a substantial burden of disease with 6.6 million mothers and 1.7 million fathers or co-parents affected by childbirth-related posttraumatic stress disorder worldwide each year. There is mounting evidence to indicate that parents who develop childbirth-related posttraumatic stress disorder do so as a direct consequence of a traumatic childbirth experience. High-risk groups, such as those who experience preterm birth, stillbirth, or preeclampsia, have higher prevalence rates." ³
Therapy is a great place to start - but it isn’t the only path to recovery. Building a sense of community is also important, whether through support groups, meet-ups, or simply having a friend to text at 3am who is going through the same life stage as you. You deserve to feel seen, validated, and supported as you navigate through this journey toward healing and hope.
For more birth-trauma resources, support, and self-care tips visit https://preeclampsia.org/birth-trauma-resources.
Follow along with us at: @maternaltraumasupport
Authors:
Co-president of Trauma-Informed Maternal Health Network
References:
¹ Leinweber J, Fontein-Kuipers Y, Thomson G, Karlsdottir SI, Nilsson C, Ekström-Bergström A, Olza I, Hadjigeorgiou E, Stramrood C. Developing a woman-centered, inclusive definition of traumatic childbirth experiences: A discussion paper. Birth. 2022 Dec;49(4):687-696. doi: 10.1111/birt.12634. Epub 2022 Apr 11. PMID: 35403241.
² Center for Substance Abuse Treatment (US). Trauma-Informed Care in Behavioral Health Services. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2014. (Treatment Improvement Protocol (TIP) Series, No. 57.) Section 1, A Review of the Literature. Available from: https://www.ncbi.nlm.nih.gov/books/NBK207192/
Related Articles

Your story is needed to improve outcomes for moms like you. Add your voice to critical preeclampsia research to ensure that every story is heard.

Doulas can help bridge the gap for any mom, but especially those most vulnerable to maternal illness and death.

Frequently asked questions about the Preeclampsia Registry, a patient-driven registry and biobank.

The Preeclampsia Foundation offers research funding, study recruitment, and other patient engagement services to researchers.

Recent findings in preeclampsia research have shown that preeclampsia likely has at least two variants – an early onset and a late onset variant. Early onset is typically defined as before 34 we...
Preeclampsia is a pregnancy complication marked by new-onset high blood pressure and signs of stress on organs such as the kidneys, liver, and brain. While much attention is often given to preterm dis...

Preeclampsia is a serious problem that can happen during pregnancy. It often affects the brain and can cause headaches, vision problems, strong reflexes, and seizures (called eclampsia). In this study...

Pregnancy offers a unique window into a woman’s future heart and cardiovascular health. Conditions such as hypertensive disorders of pregnancy (HDP) which include gestational hypertension, preec...

Heart disease, also called cardiovascular disease (CVD), is becoming more common in young women across the United States. Hypertensive disorders of pregnancy (HDP) is a group of conditions that includ...

