
Early Pregnancy Blood Pressure Patterns Can Help Predict Future Hypertension
A new research study suggests that blood pressure changes during the first 20 weeks of pregnancy—called blood pressure trajectories—may give providers a peek at a woman’s risk of developing high blood pressure years after pregnancy.
Heart disease is the #1 cause of death for women. It's becoming more common, especially in younger women. One of the first signs of heart problems is hypertension or high blood pressure. If healthcare providers can find and treat high blood pressure early, they can help prevent serious complications like cardiovascular disease, heart disease, and stroke.
Women who experience high blood pressure during pregnancy, including preeclampsia and gestational hypertension, are four times more likely to have high blood pressure later in life. They are also at an increased risk of cardiovascular disease and stroke.
But just knowing someone had a hypertensive disorder of pregnancy isn’t always enough to predict if they’ll develop high blood pressure or heart or stroke problems later.
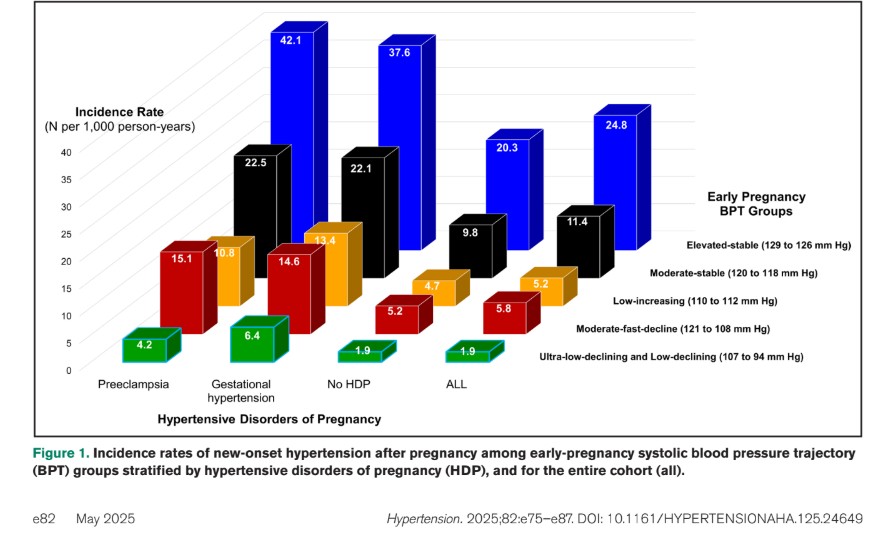
By looking at almost 175,000 pregnancies, researchers found six distinct blood pressure trajectories from the beginning of pregnancy through 20 weeks’ gestation. These early blood pressure patterns show how a woman’s body is adjusting to the changes of pregnancy. They can also help predict who might develop new high blood pressure, also known as new-onset hypertension, years later.
Studying how blood pressure changes in early pregnancy may help doctors better understand a woman’s future heart health.
What Was Studied
Researchers wanted to learn if the way a woman’s blood pressure changes early in pregnancy can help predict if she might develop high blood pressure (called hypertension) later in life. They hypothesized that early-pregnancy blood pressure trajectories would reveal a higher risk of hypertension after pregnancy in both women with and without a history of HDP. To test this, researchers looked at data from over 174,000 women between 2009 and 2019. They were healthy before pregnancy and did not have high blood pressure, heart, kidney, nor liver problems.
What They Found
- The study shows that the using the blood pressure trajectories in the first half of pregnancy in addition to other patient risk factors was able to identify differences in risk for later hypertension among women with and without a history of hypertensive disorder of pregnancy. This study was able to identify a new high-risk group among those without a hypertensive disorder of pregnancy that was like women with one.
- A woman’s pattern of blood pressure changes early in pregnancy can help predict if she’ll get high blood pressure later—up to 14 years after giving birth.
- Women whose blood pressure started higher and did not change or increased quickly during the first half of pregnancy were at greatest risk of developing high blood pressure during and beyond pregnancy, especially if they developed a hypertensive disorder of pregnancy.
Women were classified into one of six blood pressure groups based on how their blood pressure changed in the first 20 weeks of pregnancy. Women who maintained the highest blood pressure levels and those with increasing blood pressure had the greatest risk of developing high blood pressure after pregnancy compared to the women whose blood pressure was lower or decreasing. This was true for all women, but the risk was even greater for those who had pregnancy-related high blood pressure (like preeclampsia or gestational hypertension). Even women without a hypertensive disorder of pregnancy were more likely to develop high blood pressure years later if their blood pressure pattern in early in pregnancy was higher.
These blood pressure patterns can help doctors group women by risk so they know who might need more follow up care or referrals to cardiology.
Why It Matters
Doctors could use early pregnancy blood pressure patterns to:
- Spot women at higher risk for heart problems later in life.
- Watch those women more closely after pregnancy.
- Help prevent heart disease by starting healthy habits or treatment early.
Take home message:
How blood pressure behaves in early pregnancy can say a lot about future heart health.
Early pregnancy blood pressure patterns can help stratify who has the lowest to highest risk of getting high blood pressure later —even for women who had different types of pregnancy-related high blood pressure or did not develop these disorders.
When doctors look at both early pregnancy blood pressure changes and whether a woman had developed a hypertensive disorder of pregnancy, they could possibly make better predictions about her risk of heart disease over the next 10 years. Future research is needed to test this possibility.
Link: https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.125.24649
Citation: Roberts JM, Alexeeff SE, Sun B, Greenberg M, King A, Nguyen-Huynh MN, Go AS, Gunderson EP. Early Pregnancy Blood Pressure Trajectories and Hypertension Years After Pregnancy. Hypertension. 2025 May;82(5):e75-e87. doi: 10.1161/HYPERTENSIONAHA.125.24649. Epub 2025 Apr 2. PMID: 40171639; PMCID: PMC12003091.
ABOUT RESEARCH ROUNDUP
Each quarter, our team of science writers reviews the most current research studies related to hypertensive disorders of pregnancy and summarizes those studies of greatest interest and potential impact to our community, including research studies related to risk assessment, diagnosis, prevention, and treatment. Special thanks to our volunteer research team, including Dr. Sig-Linda Jacobson, Dr. Jennifer Mitchell, Dr. Julie Reynolds, and Amanda Yang who make Research Roundup possible, and to our Patient Advisory Council, who reviews these materials from the patient perspective.
Related Articles

Your story is needed to improve outcomes for moms like you. Add your voice to critical preeclampsia research to ensure that every story is heard.

Frequently asked questions about the Preeclampsia Registry, a patient-driven registry and biobank.

The Preeclampsia Foundation offers research funding, study recruitment, and other patient engagement services to researchers.
We provide research grant funding to advance progress towards detection, prevention, or treatment of preeclampsia, HELLP syndrome, and other hypertensive disorders of pregnancy.

Hypertensive disorders of pregnancy significantly increase your risk of developing long-term heart problems. A careful review of blood pressure elevations during and after pregnancy may assist in iden...

Hypertensive disorders of pregnancy (HDP) can affect different groups of women in different ways, and even though we know this happening, we don't fully understand why. There are many factors, like bi...

There is growing evidence that studies examining pregnancy and its complications need to start early within the pregnancy to fully understand the nature of preeclampsia. Key gestational milestones, wh...

It is known that chronic hypertension and high BMI (body mass index) are risk factors for hypertensive disorders of pregnancy (HDP). Studies documenting this risk have usually assessed blood pre...

Several biomarker tests are under development to predict or diagnose preeclampsia. While none of these tests are yet widely accepted in U.S. clinical practice, two FDA-approved tests are available in...



